If you have pressure or pain in one ear, dizziness, hearing loss, and a ringing or roaring noise—also known as tinnitus—it could be Meniere’s disease.
trigger of Meniere’s disease symptoms.
Table of Contents
What is Meniere’s disease?
Named for the French doctor who discovered the disease, Meniere’s is an inner ear disorder that affects hearing and balance.
Although Meniere’s disease can affect people of any age, people in their 40s and 50s are much more likely to experience it. This condition is considered to be chronic and there is no cure, but there are various treatment strategies that will minimize the effect on your life and relieve symptoms.
Potential causes or triggers of Meniere’s
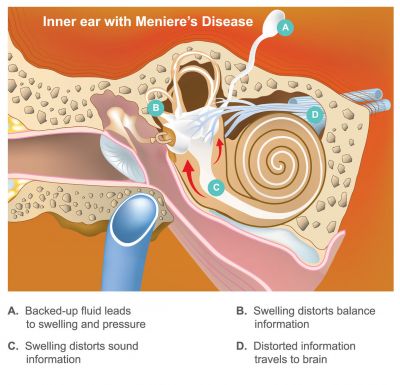
Although there is no known exact cause of Meniere’s, it most likely has something to do with increased pressure in the inner ear, which is full of a fluid known as endolymph. Another name for Meniere’s is primary idiopathic endolymphatic hydrops, which essentially means abnormal fluid in the inner ear.
Potential causes or triggers of Meniere’s disease include:
- Head injury
- Infection to the inner or middle ear
- Allergies
- Alcohol use
- Stress
- Side effects of certain medications
- Smoking
- Stress or anxiety
- Fatigue
- Family history of the disease
- Respiratory infection
- Recent viral illness
- Abnormal immune response
- Migraines
Symptoms of Meniere’s disease
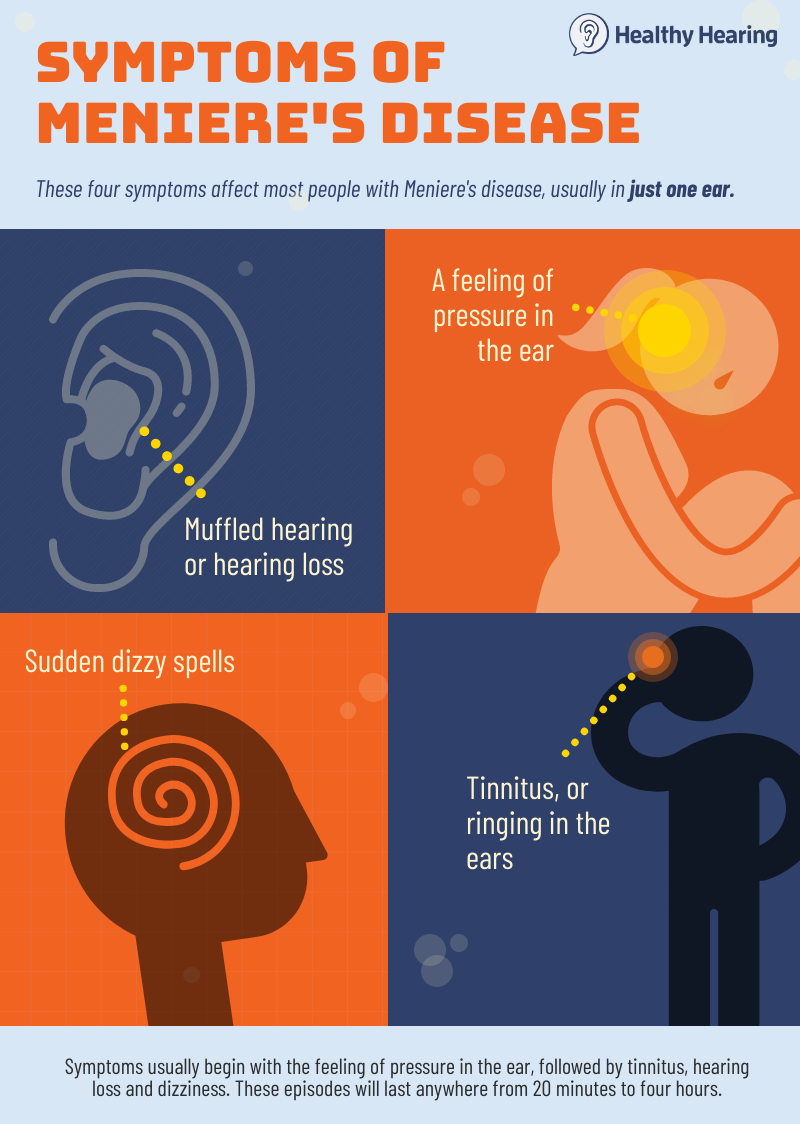
People with Meniere’s can experience:
- a feeling of pressure in the ear
- sudden dizzy spells
- tinnitus
- muffled hearing or hearing loss
Symptoms vary from person to person, and some will experience many attacks over a period of several days, and others will have an isolated attack every once in awhile. To diagnose the disease, you must experience tinnitus, hearing loss and vertigo more than once. Since all of these issues can stand alone or be associated with other diseases, Meniere’s can sometimes be difficult to diagnose. In some cases, people also experience diplacusis, known as “double hearing.”
Classic symptoms of Meniere’s include pressure in the ear, hearing loss, vertigo and tinnitus.
Symptoms usually begin with the feeling of pressure in the ear, followed by tinnitus, hearing loss and vertigo. These episodes will last anywhere from 20 minutes to four hours. People with Meniere’s will generally experience episodes in clusters with long periods of remission. When you experience an episode of Meniere’s disease, it is best to lie down and focus on one non-moving object. Often times, a sufferer will feel better after taking a nap.
Note: If your only primary symptom is vertigo, it may not be Meniere’s but instead a common condition known as BPPV.
Hearing loss with Meniere’s disease
Meniere’s disease can cause hearing loss, including mid- and low-frequency hearing loss, meaning low-pitched sounds may be harder to hear (men’s voices compared to women’s voices, or the bass in music, for example). A person also might be more sensitive to higher-pitched sounds and find them uncomfortable. However, Meniere’s disease is unpredictable and the hearing loss may not affect low frequencies, but instead high frequencies. Often the hearing loss comes and goes, making it harder to diagnose.
Some people will gradually develop more serious levels of hearing loss, which may be only in one ear or both ears. The hearing loss can range from mild to profound.
Hearing aids can generally help, since the type of hearing loss is sensorineural in origin. When hearing loss is severe, CROS hearing aids or cochlear implants may be recommended.
Stages of Meniere’s disease and diagnosis
Meniere’s disease commonly affects people in various stages, with symptoms developing over time.
- Early stage: During this time, a person will experience sudden and often out-of-the-blue episodes of vertigo that last anywhere from 20 minutes to an entire day. An person’s ear may feel blocked or full, and they may have some hearing loss, which typically goes away after the episode fades. It is also common to feel the effects of tinnitus.
- Middle stage: Symptoms of vertigo tend to become less severe during this stage, while hearing loss and tinnitus will increase in severity. Many people will also experience long-term remission (the disease goes away) that can last several months.
- Late stage: During the late stages of Meniere’s disease, patients will not suffer from vertigo as often, and some people will be relieved from it forever. However, tinnitus and hearing loss will likely get progressively worse, and people will likely experience unsteady balance regularly. Most people at this stage feel unstable in dark lighting conditions, for example.
One of the more frustrating aspects of this disease may be the delay in getting an official diagnosis. “It is important to acknowledge that a full and accurate diagnosis may take many months to attain,” write the authors of clinical practice guidelines published in the April 2020 issue of the Journal of Otolaryngology–Head and Neck Surgery.
That’s because doctors need to rule out other diseases that cause similar symptoms, the guideline authors note. These include autoimmune inner ear disease (a common cause of sudden hearing loss), otosclerosis, acoustic neuromas, temporal bone fracture, otosyphilis, vestibular neuritis, vestibular migraines and acute labyrinthitis. These diseases generally respond to different treatments.
Emotional impact
Along with the common symptoms of Meniere’s disease, it’s possible to suffer from depression or anxiety. Since the ailment affects hearing, you may develop fear and lose confidence to have conversations with others or at work, which can contribute to depression or anxiety. In addition, symptoms tend to pop up out of nowhere, so those living with Meniere’s can be in a constant anxious state, unsure of when an episode will occur. The good news: There are ways to face the fear of living with Meniere’s and tinnitus.
Remedies and relief strategies for Meniere’s
A variety of at-home remedies may help control Meniere’s, although none of them have been studied extensively to know if they’re effective or not.
Meniere’s diet recommendations
Dietary changes may decrease the amount of fluid in the inner ear, which can weaken the symptoms of the disease. Researchers looking at this issue concluded there aren’t any good clinical trials on diet and Meniere’s disease. The good news? These changes are worth trying because they aren’t harmful and may improve your overall health:

symptoms of Meniere’s disease.
- Reduce salt intake: Salt helps the body to retain water, so reduce intake of sodium-rich beverages and foods.
- Drink less caffeine: Caffeinated beverages can make symptoms like tinnitus worse, so it is best to decrease the amount of this stimulant in your diet.
Other lifestyle changes
- Stop smoking: Many people who suffer from Meniere’s disease and who regularly smoke report weakened symptoms after quitting.
- Practice stress management: Stress and anxiety are both linked to Meniere’s disease, but both can be a cause and symptom of the disease. Learning how to manage and identify stressors can bring relief. It also may be beneficial to try relaxation or meditation techniques.
More: How I manage Meniere’s with a low-salt diet
Medical treatments for Meniere’s
Unfortunately, many of the treatments for Meniere’s haven’t been studied extensively. The Cochrane Collaboration, which evaluates medical research, found only two treatments had any clinical trial evidence to support their use. Those are:
- Inner ear injections of gentamycin, an antibiotic, to help with dizziness. This is known as “chemical ablation.” Cochrane researchers said one study showed it work, but it increases the risk of hearing loss.
- Inner ear injections of steroids to combat inflammation. One study indicated this may be effective.
For both injections, though, more study is needed to know how effective they are, researchers concluded.
Other treatment options that have been less studied specifically for Meniere’s include:
- Medications that treat dizziness, such as antihistamines, benzodiazapenes and anticholinergics
- Diuretics, which are drugs that treat fluid retention.
- Surgery to reduce pressure and fluid in the inner ear
There are plenty of other suggested Meniere’s treatment options, but evidence is lacking for their use. This doesn’t necessarily mean they won’t work, they just haven’t been studied. These treatments include CBD, virtual reality treatment, positive pressure therapy, acupuncture and other alternative therapies.
Who treats Meniere’s?
Generally ear, nose and throat doctors, known as otolaryngologists, treat inner ear disorders. If you experience symptoms of tinnitus, hearing loss and dizziness, see your primary care doctor for a referral to an ENT physician or visit a hearing center near you. Always seek help right away if you experience sudden hearing loss.